Standardized assessments are a crucial tool for health care diagnostic structure and process. Utilizing the widely accepted SOAP format with a SOAP Note Template means that all healthcare professionals at your facility will follow the same documentation process.
Utilizing a standard SOAP Note Template allows all healthcare practitioners to perform their assessments using a known format. The healthcare professionals will find diagnostics and reference data more straightforward, knowing that the assessment process previously utilized the same methodology.
To help your facility with the SOAP notation methodology, we’ve created a standardized SOAP Note Template that healthcare professionals can use across various specializations. Follow along for a brief explanation of the template and some tips to best practices using the template and other tools to help your clinic move effectively and efficiently through your daily assessments.
Included In The SOAP Note Template
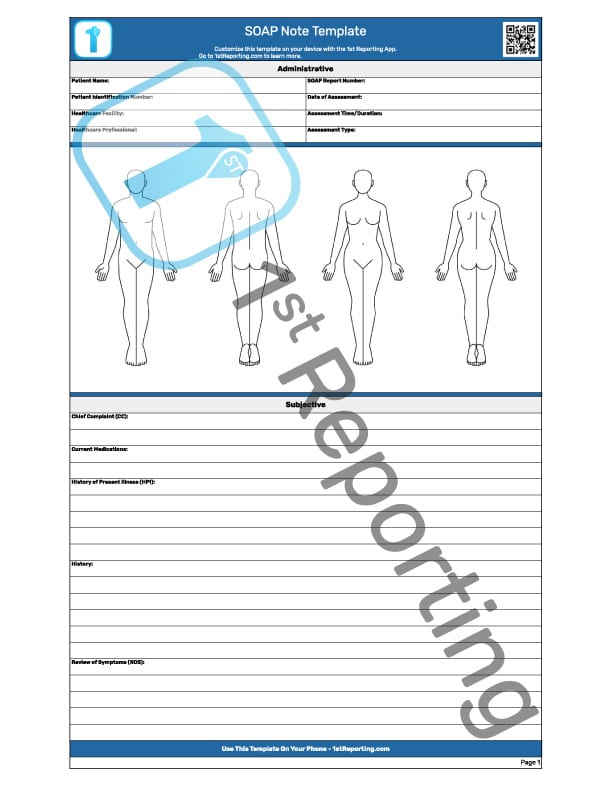
The standardized SOAP Note Template we have created is ready for various professional specializations within the healthcare industry. Please note that the downloadable version we provide does not include the watermark covering the document in the image above.
The downloadable template is a free two-page document specialized for the healthcare industry. And it has segmentation to divide the template into six easy-to-follow sections described briefly below.
- Administrative
- Subjective
- Objective
- Assessment
- Plan
- Notes
Administrative
The healthcare professional or administrative staff may complete the specific administrative information in this preliminary segment of the SOAP Note Template. Patient name and identification, healthcare provider, date, report number, and more are quickly captured by the person initiating the report.
Subjective
Following the SOAP reporting methodology, the first segment following administrative is the Subjective information section. This section includes areas to record things like:
- The chief complaint (CC) of the patient
- Current medications the patient is taking/prescribed
- A brief recent history of present illness (HPI)
- General patient history
- Review of symptoms (ROS)
It is vital to include all information provided by all professionals and the patient themselves. Some data may seem irrelevant at the moment, but for a clear view of the patient’s situation, all data needs documentation, from the CC to the HPI and ROS. (source)
Objective
The objective segment of the SOAP Note Template includes areas for the professional to record their findings of the examination, imaging, blood tests, or other diagnostic test results. Furthermore, the healthcare professional can include a preliminary assessment based on the complete view of all diagnostic information presently available. This initial assessment allows for a more transparent overall review following these sections of the objective segment:
- Patient vitals
- Patient exam details
- Imaging information
- Further patient diagnostic data
- Review of other assessments completed by other healthcare professionals
Assessment
The assessment section of the SOAP Note Template includes two areas for information documentation:
- The Problem
- The Differential Diagnosis
The Problem(s) – This section allows the healthcare professional to document (and typically list by order of severity) the patient’s problems.
The Differential Diagnosis – As the name would imply, the section allows the healthcare professional to document their diagnostic findings.
Plan
As every healthcare professional familiar with the SOAP note-taking process knows, our final part of the acronym is the plan for patient recovery or management. Each differential diagnosis should result in a treatment plan included in the SOAP assessment report section. (source)
Notes
The final documentation segment of the SOAP Note Template is the general notes section. This area allows the healthcare professional to document any further notes or information not previously recorded on the document.
How To Use The SOAP Note Template

The concept of the SOAP note method is clear: To define a standardized process of documentation of healthcare assessment. The process creates a uniform methodology widely accepted in healthcare as a leading methodology for performing rapid and non-rapid patient assessments.
The best practices of use for the SOAP Note Template are relatively straightforward. The initial step is to recognize the need for uniformity and a desire to follow industry-standard procedures within your facility. You’re here, so we’ll assume that you get that step already.
Next, you merely download the free SOAP Note Template from this page (look for the button under the watermarked image of the template). You’ll also find a link to this page found in our template library.
You will want to make enough copies following your initial download to cover the total amount of assessments you need. We recommend printing an extra few documents for each healthcare professional to review and keep in case of an error on the first few examinations.
You can now understand an initial issue with using a printed document: mistakes in permanent ink are nearly impossible to erase. So, how do we fix this dilemma? Let’s take a look at some of the tips below to find an answer to this issue. And maybe we can provide a few more solutions to common problems you might face in your reporting processes.
10 Tips For More Effective SOAP Notes And Assessments
We’ve gathered a few critical tips to aid you in your quest for a better reporting process. These tips revolve around the SOAP methodology process, so let’s dive right in.
Use The Soap Note Template As Intended.
Documentation of healthcare assessment should be rapid and standardized using the SOAP note process. This process is an industry-standard, and your facility should adopt it as a standard practice.
Follow Your Facility’s Policies And Procedures For Soap Note Documentation.
This method will ensure uniformity and compliance with industry-wide accepted practices. When your facility already has procedures in place, you can quickly adapt a customizable solution like the 1st Reporting app to your facility’s processes.
Train Everyone.
Make sure all healthcare team members use the SOAP note process to document their findings – This will create a complete patient record and allow for more accurate diagnosis and treatment. It will ease the workflow of all facility staff with a uniform process all can adopt and easily follow.
Make It Legible.
Use legible handwriting (or type) when completing the SOAP note template – This will improve the accuracy and legibility of the document. The healthcare industry is known for its illegibility. Try switching to a digital reporting platform like a mobile form automation application. Using technology eliminates the loss of information in the attempted translation of lousy handwriting.
Always Review
Review completed SOAP notes for completeness before filing or transmitting to another healthcare professional – The goal of SOAP note documentation is to provide a full report of patient assessment. Errors can lead to misinterpretation or misdiagnosis.
Always Complete, Never Partial
Ensure SOAP notes are only submitted when complete – This will ensure that SOAP notes contain all pertinent information and do not miss any vital data.
Customize Your Templates
Use custom SOAP templates created on the 1st Reporting application. This platform allows professionals to sync their assessments on a mobile, secure platform. The customization features mean creating a perfect template for your exacting needs.
Print Enough Copies (Plus Extras)
Keep in mind that when team members use a new form for the first time, they are likely to make mistakes and want to re-write the document. For this reason, ensure you’ve printed enough copies to account for mistake correction and re-writes.
Format First
Use a SOAP note template that is correctly formatted and easy to read – This will improve the efficiency of the SOAP note-taking process.
Erase Or Re-Write
Use an erasable pen when completing SOAP notes – To correct any mistakes, healthcare professionals should use an erasable pen when filling out SOAP note templates. Erasable pens can be difficult to come across. And depending on the ink used to print the template, the erasing process might muck up your paperwork.
A more straightforward and more progressive solution is to forget about having to erase at all. Or print, for that matter. Try a digital reporting solution like that offered by 1st Reporting. Mistakes are easy to fix in a digital format. And there’s no need to answer any more calls about what the writing says either.
Include some of the automation features like customized notifications, and you’ve got a winning solution to say goodbye to that printer, ink, paper, filing cabinets, and headaches.
Final Thoughts
We hope you found the template and these tips helpful in streamlining your SOAP note-taking process and creating more effective assessments! Remember, using a SOAP note template is only one part of ensuring accurate and complete documentation. It’s essential to follow your facility’s policies and procedures for SOAP note documentation to maintain uniformity throughout your organization. As always, if you have any questions about our mobile reporting solutions, please don’t hesitate to ask. We would be more than happy to help!