Healthcare professionals often have to deal with the challenge of taking SOAP notes. The problem is that many healthcare professionals lack the necessary training to take a good SOAP note, leading to errors in diagnosis and treatment. It leads to increased risk for patients and higher costs for hospitals.
We have created an easy-to-follow guide on writing better SOAP notes. Our guide will help get the documentation done quickly and efficiently while avoiding common mistakes other healthcare providers make.
What Is SOAP Notes? S.O.A.P. – An Acronym For A Methodology
Subjective, Objective, Assessment, and Plan notes (SOAP) documentation methodology is a powerful documenting method used by healthcare professionals in a vast array of specialties. Understanding the SOAP documenting the process is essential to today’s healthcare workers, managers, and professionals.
SOAP notes are a means for healthcare professionals to assess, diagnose, and treat patients using a standardized and widely accepted methodology.
- Subjective – A detailed description of the patient’s complaint, comparative history, general history, and a review of their present symptoms.
- Objective – The objective section of the SOAP includes the objective data collected by physical and observational means. This data may consist of vital signs, laboratory results, bloodwork, imaging, or other diagnostics data accumulated.
- Assessment – The assessment is the healthcare professionals’ summation of their opinion based on the findings of the subjective and objective sections of the assessment documentation.
- Plan – At the end of the assessment, the healthcare professional creates a plan of action to address the primary complaint and other subsequent issues revealed in the evaluation.
Naturally, the above descriptions are pretty ambiguous, and further explanation is warranted. We will cover each item in the SOAP note method in the following sections.
Subjective
The subjective information recording in a SOAP note refers to the patient’s history. This section should include a chronological order of patient complaints, current symptoms as disclosed by the patient, current medications, and recent medical history. Professionals might also include long-term medical history relevant to the current assessment. (source)
Objective
All healthcare professionals understand an objective viewpoint when dealing with patient complaints, issues, and assessments. The aim of the SOAP concept should include some of, if not all, of the following.
- Patient vitals information
- Patient exam findings and details
- Imaging information
- Laboratory workups
- Further diagnostic information
The concept of the objective section is the inclusion of facility and test information regarding the patient. For example, it could include bloodwork, x-rays and other diagnostic imaging, specific test results, or even previous SOAP note summaries from an earlier related visit.
Assessment
According to the National Center For Biotechnology Information, the function of the assessment section of the SOAP includes the diagnostic synthesis of information gathered in the subjective and objective segments.
The assessment should include the problem or a list of the issues displayed by the patient. Each of these problems must consist of a differential diagnosis to proceed to a planned approach to treatment.
Plan
For the healthcare professional, the goal is always to create a patient’s treatment plan. In order to achieve this final and critical stage, the professional must objectively assess the subjective and objective sections of the SOAP note. Following the assessment, the plan is formulated based on the particular needs of the patient’s situation. Each plan will be different, and rarely are two the same.
Four fundamental concepts require fulfillment in the SOAP plan segment, according to the NCBI:
- If further testing is required, one must include it — additionally, the healthcare professional’s rationale to resolve any diagnostic ambiguities that might arise.
- If therapy is required, the treatment needs inclusion in the plan for the patient. This therapy may include anything from medication to physical therapy, in essence, any therapeutic treatment.
- If a specialist referral is required, the information must also find itself included in the written plan for the patient.
- Patient education, counseling, or similar have a place for documentation in the plan. Healthcare professionals often neglect this stage, and many would be wise to remember to include proper patient education or counseling. Patients often make critical health choices based on their information, so furthering the patient’s understanding of their condition should always be included in the treatment plan.
SOAP Note Taking Best Practices
Some of the best practices were already mentioned, like the patient education portion of the treatment plan. However, we have several other best practices and tips to help facilities make some critical improvements. These improvements might aid a facility in:
- Improving patient care wait times
- Increasing positive patient care via standardized procedures
- Improving patient assessment times
- Streamlining reporting processes
Let us get right into the best practices to get started.
Use A Structured Format
A structured format makes it easier for readers to understand what they are reading without carefully reading every word or sentence. It is much more efficient to quickly scan a document and get the gist of what is going on.
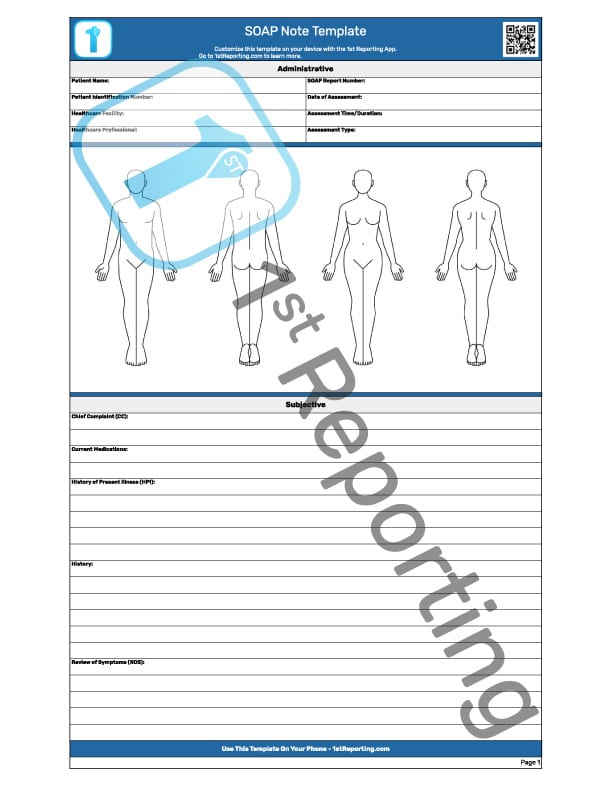
Having a standardized SOAP template is a great way to adopt a structured format within a facility. It also facilitates the standardization of assessment methodology making for a more streamlined and organized assessment process.
Use Clear, Concise Language
It is especially essential when writing SOAP notes, as clarity and conciseness ensure that everyone who needs to understand the documentation can do so easily.
Avoid Excessive Medical Jargon
Jargon and technical language limit the accessibility of documentation by those who might not be as familiar with those terms.
Be Clear
Ambiguity can make it more difficult for readers to understand what is going on, resulting in confusion and misinterpretation of one’s words. Use simple language and stick to one meaning per word to avoid any confusion.
Use Active Voice
Active voice makes one’s writing more concise and easier to read. It also sounds more assertive, which can be helpful when one needs to make a strong point.
Active voice is essential when writing the plan for the patient. Information conveyed to the patient must retain its importance as well as clarity. Passive voice adds a muddying effect to information sharing and creates ambiguity. Remember tip four about being transparent. Active voice ensures one does not make that mistake.
Format Notes For Easy Reading
Use headings, lists, and other formatting features to make notes easier to read. It will help prevent confusion and ensure that readers can get the essential information quickly and easily.
Use Standard Abbreviations
Standard abbreviations make it easier for everyone to understand the documentation, as they are universally understood. It avoids any potential confusion or misinterpretation if one uses non-standard abbreviations.
Many common abbreviations are used by healthcare professionals on documentation. However, including the appropriate terms is vital to the legibility of the document. Take the EMR format for example. In many cases in EMR, vital time is saved by the use of the appropriate abbreviations. Just ensure that the appropriate terms are used for the future understanding of those who may require the document for a future assessment.
Proofread The Work
It is essential to ensure that the documentation is clear, concise, and accurate. Quick proofreading can catch errors that might have slipped past during the writing process.
Use A Template
A template for SOAP notes can help the document process move quickly and efficiently. Furthermore, it can also help standardize documentation, improve its quality, and decrease the amount of time it takes to complete all necessary documentation. Creating a template will also help increase consistency and reduce ambiguity and errors in understanding.
If looking for a template for any portion of one’s business, facility, or industry use, look at our library of free and downloadable templates here.
Alternatively, if a digital template, like a mobile form automation app, is more the speed, try investing a few moments to find out what the 1st Reporting app can do.
The Problem With The SOAP Method And A Solution
One of the most apparent issues with the SOAP methodology is its inability to track over time. And that is despite being a standard. The concept of the SOAP methodology is practical and effective. Yet the method presents the idea of a current assessment and does not include a predominant tracking over time concept.
So, how do we create a more uniform method that can track changes over time? Perhaps a reporting system that can create various reports based on previous report frequency and other metrics?
This tracking issue over time is evident when a SOAP template used for documentation is a printed medium. Only a digital medium has the benefit of reporting and monitoring over time. Furthermore, a digital reporting solution offers security. It also offers flexibility to review and retrieve previously created documents from multiple locations easily. That means that if you operate within a multiple facility framework as many health care professionals do, you can access your documentation, reports, and so forth from any of the locations where work takes place.
Ready for a change? Try the 1st Reporting app and find the solutions you were looking to find.