Bloodborne pathogens safety must be a primary concern for organizations. Encountering biohazards in your place of business is something not to be taken lightly. If your company has taken on operations that come in contact with human blood, or you’re new to dealing with bloodborne pathogen threats within your organization, then you’ve come to the right place.
Bloodborne pathogens are those dangers to human health posed by exposure to blood or blood-contaminated items carrying dangerous micro-organisms. Potential blood exposure operations require training staff and proper personal protective equipment.
Regardless of country, the safety precautions required for needlestick or any other form of blood contaminant prevention remain the same. However, there may be slight variations in the required procedures, depending on where your organization is operating.
In this guide, we’ll go over some of the basic concepts used to establish team member safety for bloodborne pathogens. We will discuss the types of safety precautions your organization needs to implement. We’ll also provide three tips your organization would do well to implement. Let’s get started.
The Three Accepted Types Of Bloodborne Pathogens Safety Precautions
If your organization is just setting up your worker protection program, understanding the basic concepts behind mitigation and prevention is vital to the successful exposure control plan (ECP) that your business must have in place.
Universal Precautions (UP)
Universal exposure precautions assume that any potential exposure is severe, including dangerous pathogen exposure. This assumption is based on principle, not actual evidence of dangerous pathogens, but the assumption that they are always present. Therefore, each potential exposure event must be treated as the most serious and severe of events.
Standard Precautions (SP)
Standard precautions are similar to universal ones, assuming the potential risk. However, the standard precautions include normal activities that may not necessarily apply to bloodborne pathogen exposure in particular but may include other forms of exposure. These standard operational precautions might include things like using PPE (like a fresh pair of gloves per patient if in a healthcare facility, for example) for daily operations.
SP also deals with things like the maintenance of equipment in exposure environments and other similar potential exposure situations.
Transmission-Based Precautions (TBP)
The transmission-based precautions are more specifically dealing with alternative means of pathogen transmission. The alternate forms of transmission may include vapor and droplet transmission and other similar methods. The TBP protocol may not necessarily deal directly with bloodborne pathogen transmission, but depending on your operations, it may still be a requirement.
Regardless of whether or not your organization needs to include TBP protocol, one thing is certain – your organization needs to implement an Exposure Control Plan (ECP).
Implementing Your Exposure Control Plan
The first and likely most vital step to controlling the risk of occupational exposure to bloodborne pathogens is implementing a concise exposure control plan, or ECP, as it is also called. Adding this to your already existing health and safety policy is necessary and often legally required.
What To Include In Your Exposure Control Plan
Aside from some mitigating processes, several things must find their way within the Exposure Control Plan (ECP).
According to the OSHA, the ECP needs to include the following:
- A list of job classifications where all workers have occupational exposure
- A list of job classifications where some workers may have plausible exposure risk
- A list of tasks and processes which may result in the exposure risk
- Instructions and policy for determination of team member exposure
- The procedures for implementation of methods of exposure control including:
- Universal exposure precautions
- Engineering and work practice controls
- Personal protective equipment (PPE)
- Housekeeping and maintenance
- Hepatitis B vaccination
- Post-exposure evaluation and follow-up
- Communication of hazards to employees and training
- Recordkeeping
- Procedures for evaluating circumstances surrounding exposure incidents
If you’re just creating your ECP now, you can see an OSHA example of an ECP that you could copy here on the OSHA official documentation. Let’s look at each of these items in a little more detail for clarification purposes. The first four items on the list are relatively easy to understand, so we’ll go ahead and start with universal exposure precautions.
Universal Exposure Precautions
Also known as Universal Precautions, or UP, one of the most widely accepted mitigation practices regarding bloodborne pathogen exposure at work is the acceptance of universal exposure precautions.
Through the adoption of universal exposure precautions, an organization can maintain the strictest of safety protocols, maximizing staff and visitor safety.
Engineering And Work Practice Controls
Including the ECP’s engineering and work practice controls is essential for a complete and concise pathogen avoidance program. Although simple by definition, this is an essential, if not critical, inclusion in the ECP as it outlines the mechanical and process-oriented controls that your organization has implemented to mitigate blood pathogen exposure events.
Personal Protective Equipment (PPE)
Another easy-to-understand inclusion, the personal protective equipment, is included in the ECP as a means of documenting the physical controls that are worn by team members and visitors to avoid a potential exposure hazard.
Housekeeping And Maintenance
Similar to how PPE is an extended description of the physical controls in place, the housekeeping and maintenance of your facility should include the specific protocol for:
- Cleaning areas of potential bloodborne pathogen exposure
- Maintaining cleaning equipment via specific means of sanitization or other required processes for multiple-use tools and equipment.
Hepatitis B Vaccinations
In work environments where exposure to bloodborne pathogens such as Hepatitis is high, it may be necessary to implement a Hepatitis B vaccination policy. Consult your local authorities before implementation to find out what the legal requirements are in your region.
Post-Exposure Evaluation And Follow-Up
For obvious reasons, it isn’t enough for an organization to merely mandate mitigation policies. With potential bloodborne pathogen safety risks, organizations need to include post-exposure evaluation and follow-up protocol as part of their ECP.
Hazard Communication and Recordkeeping
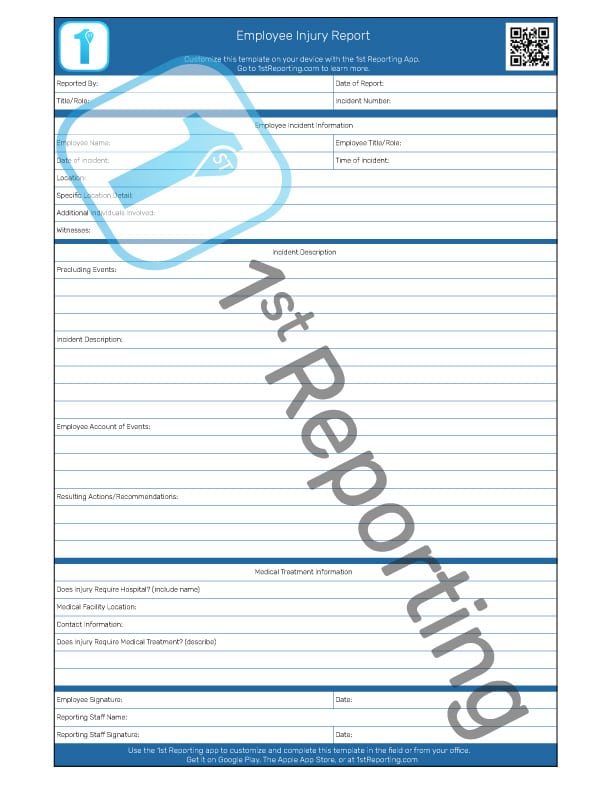
Hazard communication and recordkeeping are both vital for an effective health and safety program. Warning staff of high-risk areas or zones is essential in maintaining their safety. And recordkeeping is essential for tracking incidents from near-miss situations to team member exposure events. Tracking this information, being so critical, is best completed using a type of mobile form automation platform like 1st Reporting. Utilizing modern technology makes recordkeeping simple and effective.
Evaluation Protocol
Lastly, you must include an evaluation protocol for those situations where an exposure hazard presents itself. Whether the hazard resulted in actual or potential exposure, proper evaluation of the incident, including documentation, is the only way organizations can effectively improve safety procedures.

Exposure Plan Updates – Keeping Your ECP Up To Date
Your exposure plan must be updated annually, at the very least, if your organization operates in the United States. The plan should include updates to tasks, processes, and updates regarding new technologies that may help reduce or even eliminate risks.
Another annual inclusion in your ECP is the addition of documentation regarding input from your front-line workers. Each year, or even semi-annually, you need to canvass your staff for feedback about identifying, evaluating, and implementing new technologies or processes that they find would decrease or even eliminate exposure risks. In this way, your organization can constantly improve your safety protocol and thus continuously lower the risk exposure.
Implementing Team Member ECP Training
Second in importance only to creating an ECP is implementing it. And how do organizations achieve this feat? Through training and refresher procedures, that’s how.
Training your staff will require understanding which staff are in the greatest need based on exposure potential. Those with the greatest potential risk need training before those with the least risk.
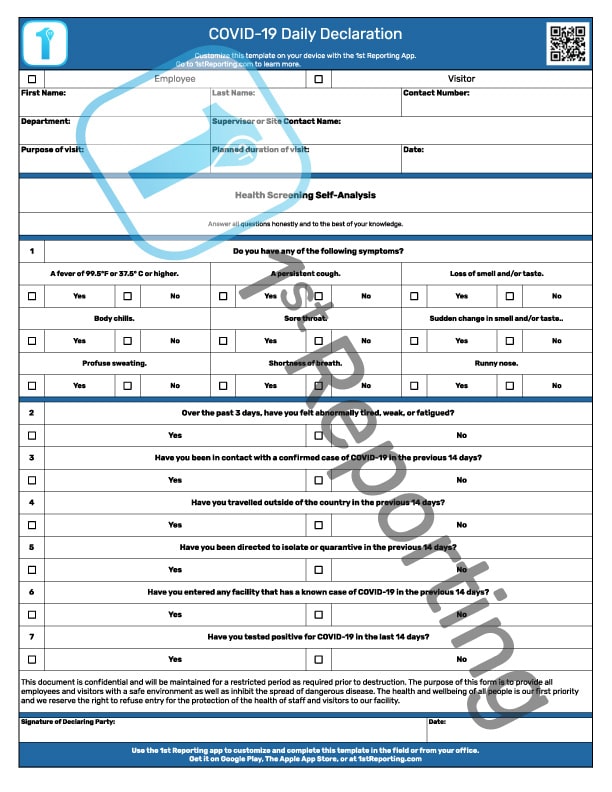
Similarly, staff must be aware of any exposure or even potential exposure documentation and reporting procedures. Whether you’re using a downloadable template that you print and complete manually or a more effective solution, like a mobile form automation app like 1st Reporting, training staff on how to deal with and react to bloodborne pathogen exposure incidents is vital to documentation, tracking, and hazard communications.
3 Tips For Effective Bloodborn Pathogen Safety And ECP Management
- When In Doubt, Use The Universal Precautions
- Implement Refresher Training
- Use Digital Reporting Software
When In Doubt, Use The Universal Precautions
We cannot stress enough the importance of the UP protocol. Following this methodology will incur extra costs in labor and PPE. Still, the costs vastly outweigh the potentially fatal exposure incidents that are more likely to occur when the UP protocol is not implemented.
The universal exposure precautions methodology is literally life-saving. Don’t ignore it in your organization.
Implement Refresher Training
It is nearly common knowledge from the plethora of studies and papers on human memory retention that repetition increases memory retention. With an increase in training refresher frequency, we can find that optimal training memory retention might be achieved by team members.
Some organizations only pursue refresher training at the minimum legally required schedule. However, in the interest of safety, it is smart for any management team to implement a more frequent schedule of mandatory staff refresher training.
Use Digital Reporting Software
If the level of risk exposure is so low that you could likely get by with only a few copies of a form, then downloading a free template is likely a decent enough solution. However, if your business or organization is growing, reporting using multiple forms, checklists, or others, or if you want to report events digitally, you need to investigate a digital reporting solution. May we be so bold as to introduce you to 1st Reporting?
1st Reporting offers a mobile form automation solution for all of your reporting needs, from near misses to team member injuries. With a wide variety of pre-built templates and an easy-to-use custom form creator, your organization can do away with the filing cabinet and clipboard and get digital.
Using a mobile reporting solution app like 1st allows your organization to unplug the printer, get rid of the filing cabinet, and moves your efficiency up more than a notch with automated processes that simplify your incident management tenfold.
Custom notifications are a great feature that allows your business to set up automation. When a team member completes a blood pathogen exposure report, the system can send an automatic notification to the appropriate manager the moment the report is submitted. And as long as that manager has a login to the app, they can access that same report from another location.
Final Thoughts On Bloodborne Pathogen Safety At Work
Understanding how your organization will implement the three precautionary methodologies (UP, SP, TBP) into your ECP is vital to your health and safety program’s success in dealing with bloodborne pathogens and their exposure potential.
Including the proper items and information within the ECP is equally critical to the implementation of the ECP and the use of its required protocol and practices.
Finally, utilizing proper training, recordkeeping, and a robust reporting solution like 1st Reporting is a surefire way your organization can lower risk exposure for staff, visitors, and the organization itself. Give 1st Reporting a try in your organization and see the difference in efficiency a little mobile form automation can make.